Announcements
Some Users Experiencing Availity Issues for New Members
Blue Cross Blue Shield of Wyoming has updated t he Provider Manual that contains operational policies and procedures to keep you and your staff informed. You can find it at BCBSWY.com/Providers under Provider Resources. We recommend bookmarking this page as the manual is regularly updated and the online version contains the most current information.
Find Your Remits at Availity
Providers should get their remittances from Availity. Availity is the fast and easy service option that is available when you are.
As a reminder, log in to Availity and follow these simple steps to register:
- Step 1: After Logging in Click “My Providers” then go to Enrollments Center
- Step 2: Select ERA Enrollment
- Step 3: Click Claims & Payment Ɩ Select EDI Reporting Preferences Ɩ Click Claim Payment/Advice tab.
Prior Authorization Training Webinar Available
Only one week remains to register for our upcoming virtual training session for Predictal. This webinar is designed to help you maximize your Prior Authorization workflows.
You must register in order to attend. The one-hour training opportunity will begin at noon on Wednesday, Feb. 7, 2024.
Register for Prior Authorization Webinar
Good Habits
Provider Directory Validation Tool Reminder
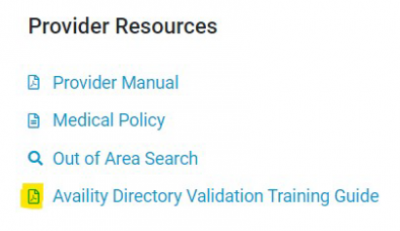
You can find the Provider Directory Validation Tool guide under the Provider Resources section on the right rail of the website.
Providers can use the Directory Validation tool on the Availity Portal to find NPI and tax ID combinations.
The No Surprises Act (NSA) requires you to confirm this information every 90 days.
Good Habits
Provider Directory Validation Tool Reminder
You can find the Provider Directory Validation Tool guide under the Provider Resources section on the right rail of the website.
Providers can use the Directory Validation tool on the Availity Portal to find NPI and tax ID combinations.
The No Surprises Act (NSA) requires you to confirm this information every 90 days.