Announcements
Some Users Experiencing Availity Issues for New Members
Some BCBSWY Availity users are experiencing membership error issues when requesting a prior authorization for members effective 1/1/2024. We are currently working with Availity to resolve this. If you encounter an error with your prior authorization request, please submit a fax to us directly to us directly at 307-432-
2917.
Prior Authorization Training Webinar Available
After popular demand, we are excited to announce another virtual training session for Predictal to help you maximize your Prior Authorization workflows.
You must register in order to attend. The one-hour training opportunity will begin at noon on Wednesday, Feb. 7, 2024.
Register for Prior Authorization Webinar
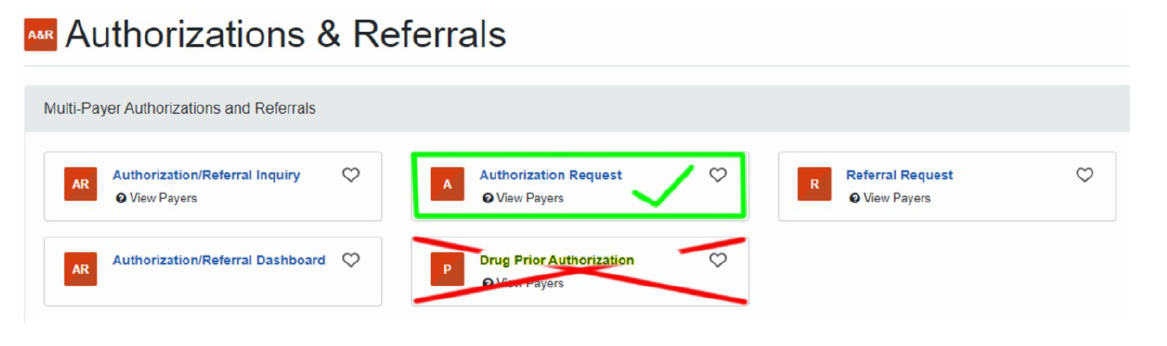
Know The Right Authorization Request
BCBSWY has received numerous questions regarding the Drug Prior Authorization box on Availity. If you see this option, please know this access is used by different payers — it is not used by BCBSWY.
All authorizations, regardless of CPT or HCPCS code, including drugs, should use the AUTHORIZATION REQUEST box.
See image below.
Digital Breast Tomosynthesis Billing Tips
BCBSWY will only reimburse Digital Breast Tomosynthesis (DBT) services billed using CPT codes 77063 and G0279. These codes represent DBT being performed as an add-on service.
The following are the four CPT codes that currently represent DBT services:
- 77061 – Digital breast tomosynthesis; unilateral
- 77062 – Digital breast tomosynthesis; bilateral
- 77063 – Screening digital breast tomosynthesis, bilateral; add-on
- G0279 – Diagnostic digital breast tomosynthesis, unilateral or bilateral; add-on
Please note: DBT services billed using code 77061 or 77062 will be denied.
Good Habits
Provider Directory Validation Tool Reminder
You can find the Provider Directory Validation Tool guide under the Provider Resources section on the right rail of the website.
Providers can use the Directory Validation tool on the Availity Portal to find NPI and tax ID combinations.
The No Surprises Act (NSA) requires you confirm this information every 90 days.