Announcements
Prior Authorization on Hearing Aids Services
Effective 01/01/2024, FEP began requiring Prior Authorization on Hearing Aids services.
To be considered as a covered benefit, prescribed hearing aids must be an FDA approved device and prescription grade. Over-the-counter hearing aids are not a covered benefit.
All authorizations must include the 510(K) number, the name and model of the hearing aid.
Submitting Inpatient Authorizations – Start of Care Date
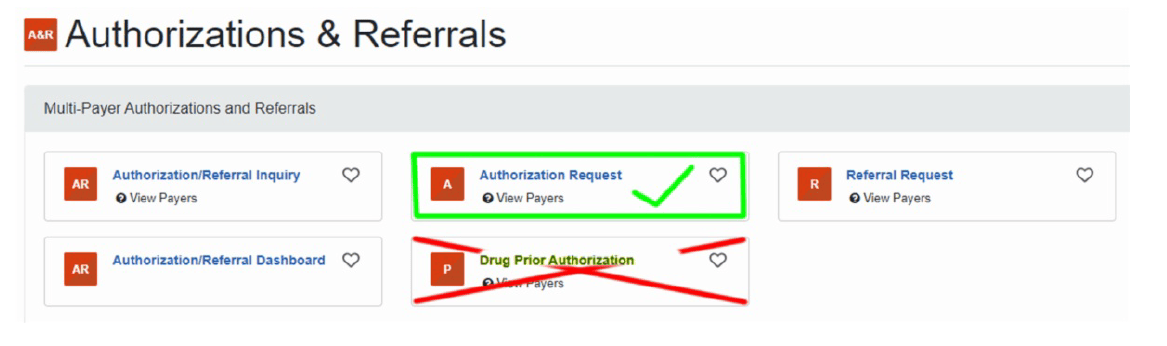
When submitting inpatient authorizations through the Availity portal, always update the START OF CARE DATE to the member’s admission date for the inpatient level of care. Otherwise, it will default to an incorrect date.
Note: This should not be the date the patient entered the facility or is in an observation status unless you are requesting an observation stay review.
BCBSWY only requires review of observations stays for Federal Employee Program (FEP) members when the observation surpasses 48 hours.
Good Habits
Provider Directory Validation Reminder
| You can find the Provider Directory Validation guide under the Provider Resources section on the right rail of the website.
Providers can use the Directory Validation tool on the Availity Portal to find NPI and tax ID combinations. The No Surprises Act (NSA) requires you confirm this information every 90 days. |
|