Reimbursement Change
Effective Oct. 1, BCBSWY will begin using J-code level pricing for J-1745 (infliximab). We will no longer be pricing this medication at the NDC code level. Reimbursement will be at the biosimilar rate.
Directory Validation Tip
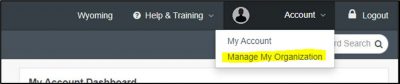
In Availity, beneath the user account, please select “Manage My Organization” to make updates. (See screenshot below.) Additional instructions are located here to help you find NPI and tax ID combinations. This helps facilitate compliance with the No Surprises Act (NSA) provider directory validation requirements. The NSA requires you confirm this information with us every 90 days, so your information can continue to be listed in our public directory.