COB Inquiry Reminder
Providers who have Coordination of Benefits inquiries, questions, or
concerns should send a fax to 307-432-2942.
Please include the BCBSWY Request for Professional or Institutional
Claim Adjustment found at BCBSWY.com/providers/providerresources/
forms/.
These inquiries should be listed under Workers Compensation, Medicare,
No Fault, Subrogation, Other Insurance.
Call for Volunteers
BCBSWY is seeking Providers and Billers to provide feedback for
BCBSWY.com/providers/. Our goal is to learn how we can improve
accessibility to the features you use most. The feedback 30-minute
session will be one-on-one with our Consumer Experience Specialist.
Sign Up Here
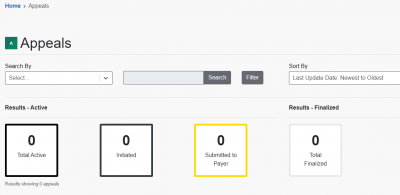
Availity Appeals Best Practices
Please note that all appeals submitted requesting a status update will be
closed. The appeals status can be viewed on the Availity dashboard. The
Dashboard can be found by going to “Claims & Payments” and then
selecting “Appeals.” Please refer to the Wyoming Availity Appeals guide
using the button below for more information.
Our Member Services Department is available to assist you with status
updates Monday through Friday, 8 a.m. to 5 p.m. at 1-800-442-2376.
Download the Availity Appeals Guide Here.